Little Ashlyn Smith is a wiggle worm on her mom’s lap, chewing on a small stuffed animal. It’s a simple sensory task that most toddlers perform, but for Ashlyn, it wouldn’t have been possible without the care of an expert medical team and surgery she underwent with Dr. Michael Jaskolka.
Ashlyn was born with a bilateral cleft lip and cleft palate, a congenital difference causing an opening in the roof of the mouth that affects the face and skull of one in 700 babies born in the United States.

“Ashlyn had difficulties breathing and eating when she was born,” explained Ashlyn’s mom, Kylie Smith. “She didn’t have a nasal cavity because of her bilateral cleft lip and palate.” Ashlyn needed to be fed using a specialized bottle lined up at a precise angle with her nose because she couldn’t create suction.
It’s common for bilateral cleft lip and cleft palate to challenge the child’s ability to breathe, eat and form speech. And for parents who learn the news from an ultrasound pregnancy scan during a prenatal appointment, it can be a scary moment to hear their baby will be born with facial differences. But Jaskolka, a cleft and cranio-maxillofacial surgeon, restores smiles in both children and their parents by supporting them physically and emotionally throughout this journey.
Jaskolka normalizes these differences when he meets with expectant parents for the first time. As medical director of the cleft and craniofacial team at Novant Health New Hanover Regional Medical Center in Wilmington, he specializes in managing cleft lip and cleft palate, facial injuries and craniofacial reconstruction.
Nationally recognized surgical treatment close to home.
A team approach to treatment and care
Since 2014, Jaskolka has directed the cleft and craniofacial team at New Hanover Regional Medical Center in Wilmington, following a similar role in Charleston, West Virginia.
Patients come from North Carolina, South Carolina and Virginia for care from Jaskolka’s multispecialty team that includes pediatric dentists; nutrition and feeding experts; genetic counselors; orthodontists; ear, nose and throat surgeons; speech and language pathologists; developmental psychology experts and social workers, along with clinical coordinators who direct the patient experience. For these efforts, the team is recognized for meeting the high standards from the American Cleft Palate-Craniofacial Association (ACPA).
A cleft lip can occur as early as the fifth week of gestation. A cleft palate can form within the first nine weeks but might not be identified in an ultrasound until later.

“I relay to the parents that it’s nothing they’ve done, that sometimes a cleft runs in the family,” said Jaskolka, a father of three himself. “It’s important to recognize that it’s normal to have difficult emotions. It can be scary, and I encourage families to talk to each other openly and even meet with a therapist or counselor.”
Smith, a resident of Rocky Point, about 30 minutes away from Wilmington, was referred to Jaskolka by her maternal fetal medicine team during her pregnancy.
“Being scared and not knowing anything about cleft lip and palate, Dr. Jaskolka and his team were always reassuring and made our family feel very comfortable during this entire process,” Smith said.
Though Jaskolka treats patients of all ages, he focuses on pediatric reconstructive surgery, which includes corrective jaw surgery and cranial, head and neck reconstruction. Along with his partners, Jaskolka cares for patients of all ages who have sustained facial injuries; recent patients include a 5-year-old child with a jaw fracture and a 72-year-old with a broken nose and eye socket fracture.
“Birth to college” continuity of care
A misconception of cleft surgery is that it is performed only to serve a cosmetic purpose. But this reconstruction is, in fact, a functional necessity that occurs in stages. It begins with lip repair as early as 4 months and often ends in the patient’s late teens, with jaw surgery and a rhinoplasty.
“There’s rarely a need to rush a child into an operation for a cleft lip or cleft palate,” Jaskolka said. “We like to let the infants grow and make sure they are healthy in order to reduce anesthesia risk.”
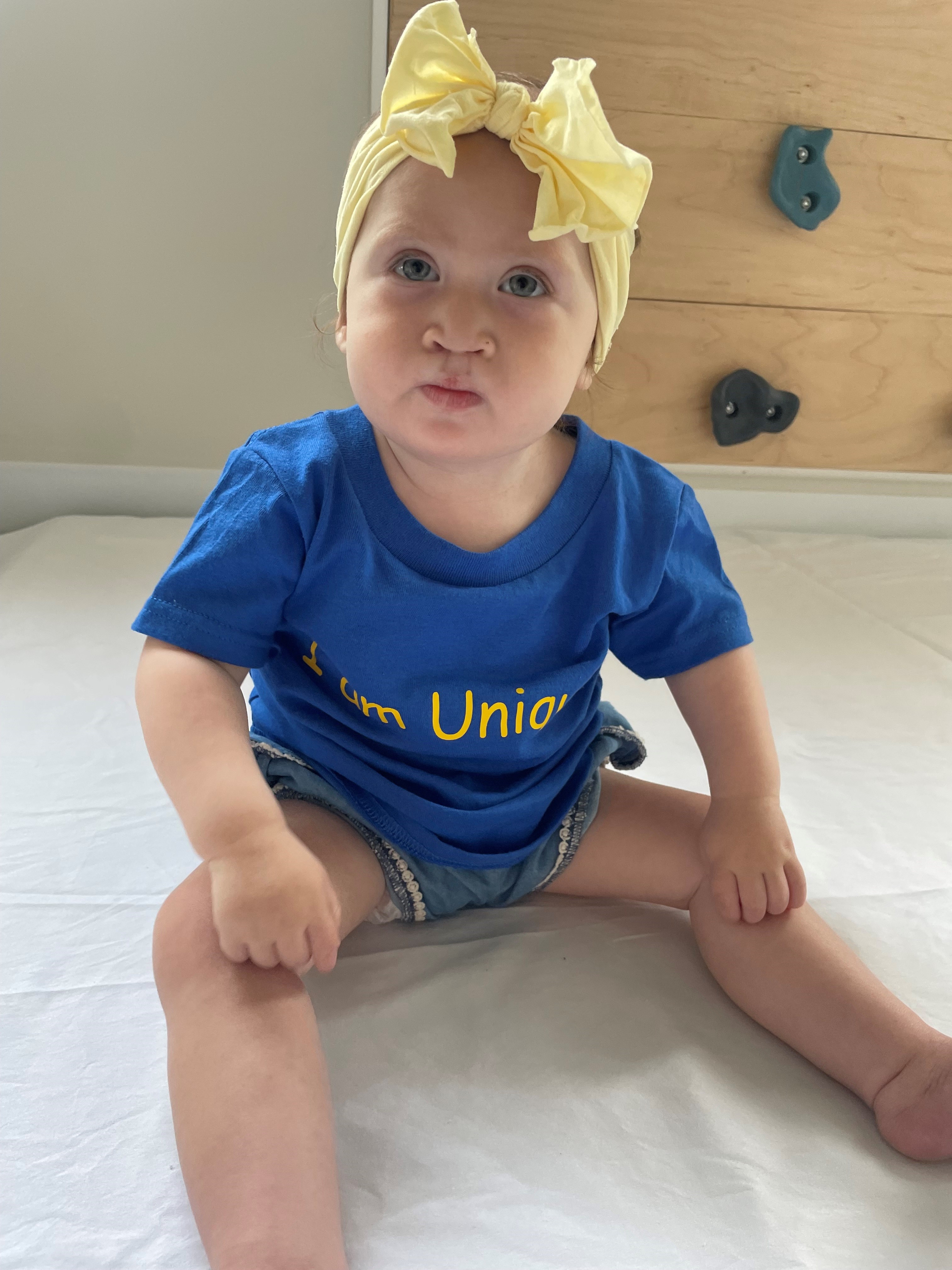
This comprehensive cleft treatment, requiring an investment of about 18 years, is what Jaskolka describes as a “birth-to-college” timeline. Depending on a child’s personal needs, routine visits include various stages of surgery, speech therapy and general care. Today, 2-year-old Ashlyn works on eating food and getting used to different textures with an occupational therapist and the feeding team at the Novant Health Nunnelee Pediatric Multispecialty Clinic.
The “birth-to-college” cleft treatment timeline includes:
- For a child with both a cleft lip and palate, Jaskolka typically repairs the lip at 3 or 4 months. This functional repair helps with nursing or taking a bottle. Ashlyn underwent this procedure at 7 months.
- The palate cannot form speech without being reconstructed, which typically happens at 9 months. Ashlyn received this surgery at 1 year and it enabled her to start using a sippy cup.
- A bone graft is often necessary for jaw reconstruction and is performed at six or seven years, depending on when the child starts to develop their adult teeth.
- Sometimes additional surgery is needed to help with speech or to align the jaws.
- A lip revision or rhinoplasty is typically performed during the teenage years, toward the end of treatment.
Caring globally
Jaskolka’s practice isn’t limited to Wilmington. Every year, he travels to Guatemala with the organization Sharing the Journey International to perform cleft surgeries. On one visit, Jaskolka operated on a 47-year-old man who then, for the first time in his life, was ready to remove the bandana that hid his face.
Jaskolka attended dental school in his native Canada, where a lecture on cleft treatment ultimately steered his interest in studying oral and maxillofacial surgery at the University of North Carolina at Chapel Hill. He finished his training by completing a fellowship in cleft and craniofacial surgery at the Arnold Palmer Hospital for Children.
“I was taken with the thought of impacting people with that type of surgery,” he said. “It’s something to feel really good about, and I love it. You get to know the families and develop that bond by being genuinely interested in doing the best you can for them and watching them thrive.”












