Helping patients regain the ability to dress and feed themselves, or just live a more active and independent lifestyle, is extremely rewarding.
Since September of 2020, more than 500 patients have had incisionless brain surgery at Novant Health to treat disabling tremor. Novant Health neurosurgeons were the first in the Carolinas to use an advanced procedure, called magnetic resonance (MR)-guided transcranial high-intensity focused ultrasound to treat thalamotomy.
The FDA also approved staged, second side treatment in December 2022, meaning patients can have tremor in both hands treated. In early 2024, Novant Health became the first treatment center in the region to upgrade to the more technologically advanced Exablate Prime system, making treatment even faster for patients.
“This technology gives a treatment option to a lot of patients who otherwise would not be good candidates to undergo — or would be reluctant to undergo — a more invasive treatment,” said Charles Munyon, MD, Novant Health neurosurgeon based in Charlotte.
“This is an option for patients who have essential tremor or tremor-dominant Parkinson’s disease that is not responding to medication and is causing significant detriment to their quality of life,” Dr. Munyon said. “They may have problems eating and drinking, playing musical instruments, writing, dressing or performing hygiene tasks. For any given patient, what’s important to them may be different, but we work with them when their tremor is getting in the way of things they want to do.”

The results are immediate, with up to 90% reduction in tremor.
“We are usually looking for 70% to 90% reduction in tremor,” Dr. Munyon said. “Sometimes we can do better. Usually that’s enough to let people go back to eating and drinking even difficult foods, regain their ability to write legibly and to do tasks around the house. Some of my patients have returned to art and even brought me a few sketches.”
There’s no incision necessary.
“We use focused sound waves to make a small hole in the thalamus where the circuitry that drives tremor is running,” said Dr. Munyon. “Because those sound waves can be transmitted through the scalp and skull, we don’t have to make any incisions. And because we’re using heat to create the lesion, we can use the MRI essentially as a thermometer. We can see where the temperature in the brain is changing, and we can make sure that it’s exactly where we want the temperature to change.”
The treatment is a low-risk, outpatient procedure.
Dr. Munyon and his team perform focused ultrasounds in an MRI suite at Novant Health Mint Hill Medical Center. Without an incision, there is no risk of infection and there is no significant risk of bleeding. Neurosurgeons perform the procedure in conjunction with MRI technicians, a physician assistant who helps with patient prep, as well as a nursing team supporting the patient before and after the procedure.
Patients may not be eligible for treatment if they are not safe to be in a 1.5 Tesla magnetic field due to an implanted device or metal in the body. “It’s important that patients who suffer from claustrophobia may have a hard time tolerating the procedure, and ease of performing the procedure may vary depending on the patient's skull,” said Dr. Munyon.
Alternative to a focused ultrasound could be deep brain stimulation (DBS).
The DBS procedure involves making small holes in the skull to place electrodes into one or two sides of the brain that will target specific areas that control movement. After this, chest wall surgery is required to place the neurostimulator under the skin in the chest.
DBS delivers adjustable stimulation that can take up to six months to find the optimal setting. The patient is given a small remote that allows them to turn the stimulation on and off, depending on the instructions given by their physician. Medicine may still be needed for certain conditions.
In some cases, where DBS might be referred, a focused ultrasound might fit the patients’ needs better. “The decision about which surgical treatment (if any) to pursue for treatment of tremor depends on a number of factors and is best left to each patient once they have been given adequate education on their options,” Dr. Munyon said.
The procedure is quick, lasting about 45 minutes.
Not only is the procedure fast, but the goal is for it to be a one-time procedure for each patient. “Some may undergo an additional focused ultrasound procedure if the effect isn’t quite as good as the team was hoping for, or if we see something that can be improved upon,” Dr. Munyon said.
Second side treatment has been approved.
“The FDA has approved staged, second side treatment, meaning that patients can have both hands treated provided that their first side treatment goes well, and nine months have elapsed between treatments,” said Dr. Munyon.
Since the FDA approval, Dr. Munyon and his team have performed more second side treatments than anyone else in the country. “The decision to have the second hand treated still requires careful attention, as a good result on the first side does not guarantee a similar outcome for the second side.”
Side effects are minimal and tend to dissipate in about six weeks.
Side effects are temporary for most patients and can include a change in taste, mild slurring of speech, numbness or tingling in the lips, tongue or mouth, and mild drifting when walking.
“There is a 3% risk of long-term side effects associated with this treatment,” Dr. Munyon said. “For most patients, this is manageable, such as discoordination or imbalance, numbness or unpleasant tingling in the face, arms, legs or lips on the side of the body that was treated.”
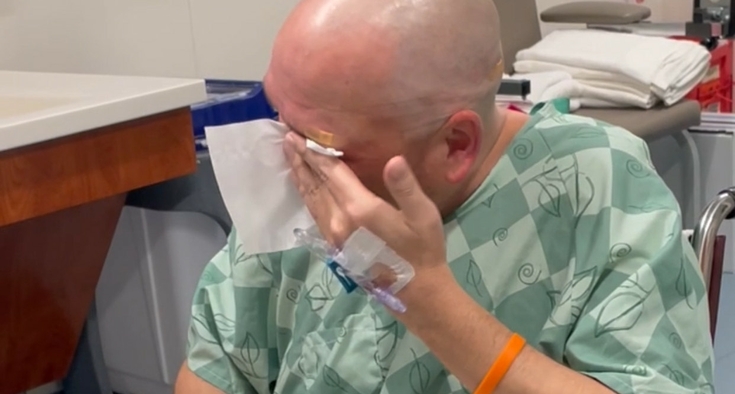
The procedure makes it possible for patients to finally return to more active lifestyles.
“Many tremor patients have suffered for years or even decades with a debilitating and progressive condition,” Dr. Munyon said. “Helping them regain the ability to dress and feed themselves, or just live a more active and independent lifestyle, is extremely rewarding.”
Charlotte Region
Novant Health Brain & Spine Surgery: 704-316-3070 Charlotte, NC