As if being diagnosed with head or neck cancer isn’t bad enough, these patients need clearance from a dentist before they can begin cancer treatment. And that could lead to extensive, and often expensive, dental work. To complicate things further, it’s often hard to get in to see a dentist if you’re not already an established patient.
If dental problems aren’t addressed on the front end, they can lead to serious complications during and after treatment. Dental infections can become much more dangerous when the immune system is weakened, as it is during chemotherapy. It’s also important to remove any non-salvageable teeth before starting radiation, which reduces the jawbone’s ability to heal. Post-radiation extractions can result in a serious condition called jaw osteonecrosis (death of jawbone tissue).
Until July, Novant Health oncologists had to engage dentists or oral surgeons in the community to do a pre-cancer-treatment exam and possibly pull teeth. The problem was: Most dentists aren’t accustomed to greenlighting a cancer patient for treatment and don’t feel confident doing it.

But Dr. Shaiba Sandhu does. In July, she became affiliated with Novant Health Cancer Institute - Forsyth, which has partnered with High Point University (HPU) to provide oral medicine care for cancer patients. Sandhu is a dentist specializing in oral medicine and orofacial pain and a clinical assistant professor at HPU’s recently launched Workman School of Dental Medicine.
The partnership is just one example of Novant Health’s efforts to remove barriers to treatment, which are often highest for people from marginalized communities with limited access to health care and dental care.
Sandhu, who completed a three-year, hospital-based oral medicine residency at Harvard Dental School, is one of only two certified oral medicine doctors in North Carolina.
Supportive care throughout your cancer journey.
Team approach

Dr. Demetria Jacks, an oncologist/hematologist with Novant Health Cancer Institute - Forsyth, said having Sandhu on the team “has really transformed the care we offer patients” by speeding up the dental work to clear the way for cancer treatment.
Sandhu is also there throughout their treatment to diagnose and manage oral side effects. “Our goal is for cancer therapy not to be interrupted,” she said. Cancer treatment can cause painful sores in the mouth that make it hard to swallow. Sandhu can help treat those.
She knows the stakes her patients are facing and works quickly to take care of their dental needs because there’s a bigger goal. “Dental issues shouldn’t be a hurdle in someone’s initiation of life-saving cancer therapy,” she said.
‘A dermatologist for your mouth’
While only recently recognized by the American Dental Association, oral medicine has been around since the 1940s, Sandhu said. She tells people she’s “like a dermatologist for your mouth, with expertise in the disorders of the mucosa (the skin) of the mouth.”
Understanding oral medicine
While dentistry is an ancient practice, oral medicine was only recognized by the American Dental Association (ADA) in 2020.
The difference between oral medicine specialists and oral surgeons is that, while “both can perform dental extractions and complete dental clearances,” Sandhu said, “oral surgeons are not trained to diagnose and manage lesions of the mouth to the extent we are.”
Oral medicine specialists provide “dental treatment exclusively for medically complex patients,” Sandhu said. “A major cohort of that is oncology patients. We ensure that all sources of dental infection are addressed before starting radiation, and we specialize in managing both short-term side effects, such as mucositis (oral sores), and long-term side effects, including dry mouth, radiation cavities, altered taste, trismus (reduced mouth opening), radiation-induced neuropathy (nerve-related pain) and jaw osteonecrosis.”
Patients with multiple myeloma and metastatic solid cancer – the kind that can spread to the bones – also get a referral to Sandhu. These patients are often started on bone-strengthening medications, such as bisphosphonates or denosumab, to slow bone loss and strengthen their bones.
“While these medications are effective in preventing bone-related complications like fractures, they can also lead to osteonecrosis of the jaw, a condition where parts of the jawbone die,” Sandhu said. “To reduce this risk, dental clearance is essential before starting treatment with bone-strengthening medication to eliminate any sources of dental infection.”
She uses this analogy to explain why seeing an oral medicine specialist (as opposed to your regular dentist) before beginning cancer treatment is a good idea: “While you could go to your (primary care clinician) to look at a skin problem, they may miss something that a dermatologist would likely catch.”
Before oral medicine, oncologists referred their patients to community dentists and oral surgeons for the clearance exam. But oral surgeons aren’t part of the hospital system – and couldn’t always do dental clearances at an expedited rate.
Sandhu can.
Before she arrived, patients often experienced sticker shock after learning about the cost of the dental work they needed. It’s rare, but some patients even decided to forego treatment entirely because of the cost of dental work.
“As a clinician, you want to go above and beyond for your patients,” Sandhu said, “but sometimes there are financial hurdles, and you wonder: What can I do to help?”
One way she can help: Unlike general dentists, she can bill patients' medical insurance for their medically necessary dental treatment.
And then some
It’s not just head and neck cancer patients who need dental clearance. Patients with blood cancers such as leukemia and lymphoma also need to be sure there’s no source of infection before their treatment, especially before stem cell transplants or chimeric antigen receptor T-cell (CAR-T) therapy.
During stem cell transplants, patients’ immune response will decrease. There may come a time when their white blood count is 0. “When patients have no immune system to fight infections, even a small source of oral infection can spread in the body and lead to life-threatening sepsis,” Sandhu said.
The mouth/body connection is clear. What happens in the mouth can impact the rest of the body. That’s important for everyone to know – but especially people undergoing treatment for head and neck cancers, blood cancers and metastatic solid cancers.
“We do a very good job of curing head and neck cancer,” Jacks said, “but people are left with real quality of life issues afterward. So, it’s vital that we work to improve people’s quality of life as much as possible.”
Sandhu is doing a lot to ensure that happens. It’s a process that’s ongoing. She said, “We're with cancer patients before, during (if any complications arise) and long after completion of their cancer therapy.”
A grateful patient’s journey
Radiation saves lives, but it also has a lifelong adverse effect on the mouth, teeth and jaw bones.
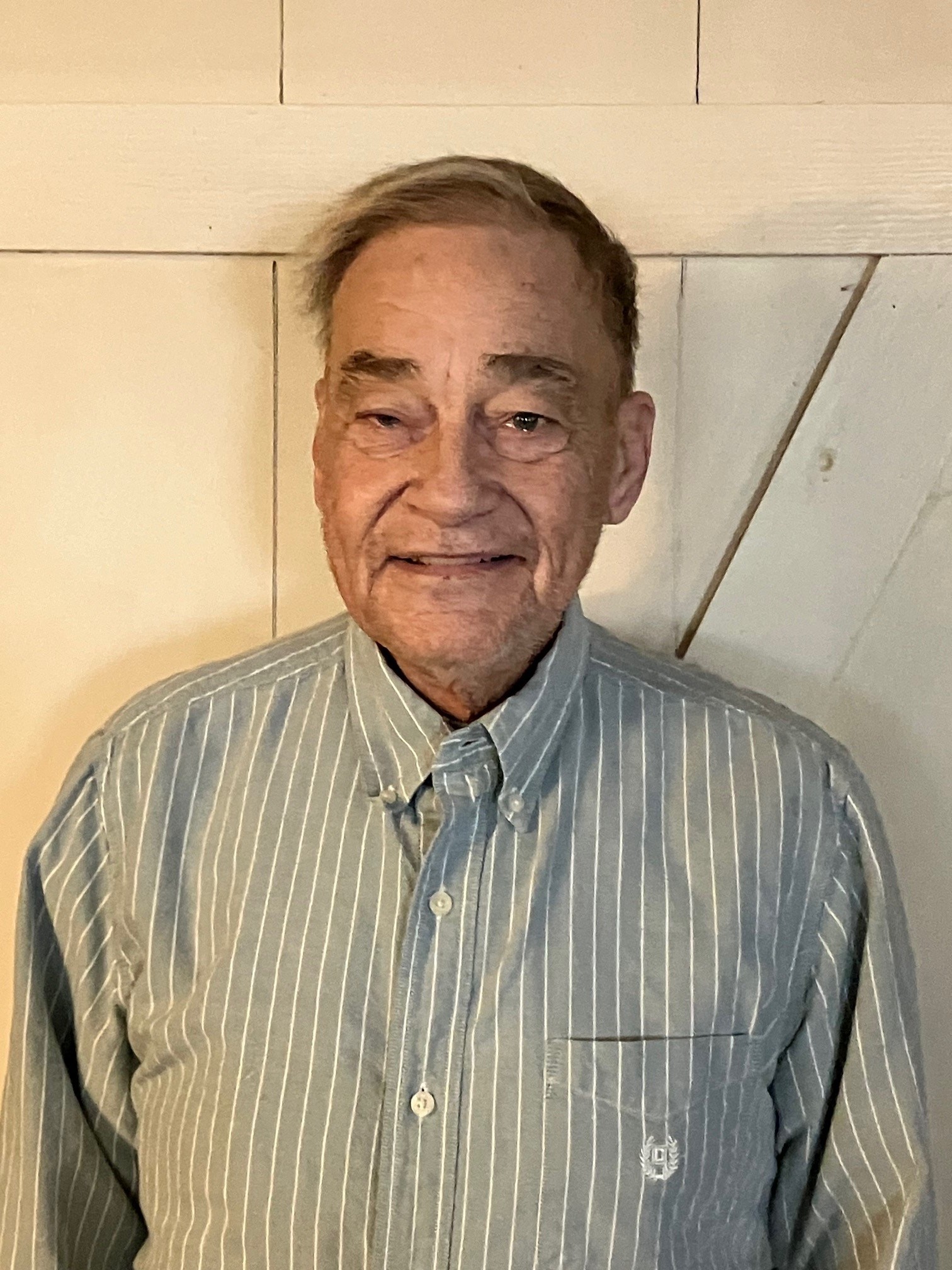
“Radiation left my teeth in such bad shape that it was hard to chew,” said Ernest Stewart, a head and neck cancer patient who’s been treated by both Drs. Jacks and Sandhu. “It’s such a nice experience to get your mouth looking good again.”
An inability to chew is more than an inconvenience. It’s frightening.
“Certain foods, I couldn’t even swallow,” Stewart said. “Salad, for instance, was very hard – unless the lettuce was torn into very small pieces. Meat was hard, too. I used to get choked regularly to the point I’d have to leave the table and go to the bathroom, which was embarrassing. It sometimes felt as if my air supply was being cut off.”
Stewart, a retired construction worker from Germantown in Stokes County, has been treated at Novant Health for three different cancers during the last eight years. He’s already exceeded the life expectancy he was given when his throat cancer was discovered in 2016. He’s no longer receiving treatment for cancer and is receiving hospice care at home.
“In order to have hospice care, a doctor has to say your life expectancy is six months or less,” he said. “But many patients – and I think I’ll be one of them – live past the six months. So, they sign you up for another six months. I’m still able to do things. I teach Sunday School and serve on a few committees at church. I have days when I’m weak and just need to stay home. But, for the most part, I do most everything I want to do.”
At 74 – and in spite of his metastatic cancer – he’s still an active outdoorsman. The Civil War buff loves to travel – Gettysburg was a recent destination – and go on deer-hunting trips every year. He took one shortly before the holidays with a group he’s been hunting with for three decades. Each year, Stewart fixes a special dish that everybody requests – a Cajun version of stewed potatoes with celery, green onions, green peppers, bacon and spices. He serves it with homemade cornbread fritters.
Best doctors. Amazing nurses. Remarkable care.
Stewart credits his survival to his care team at Novant Health and his strong faith. “Being able to trust the Lord and everyone I've dealt with at Novant has been wonderful,” he said. “There’s only so much people can do for you when you have terminal cancer, but it helps to know people are praying for you and taking care of you.”
Due to the long-term effects of radiation, Stewart developed cavities in his upper teeth and needed to have them pulled. Because of his cancer history and the risk of delayed jaw bone healing (osteonecrosis), no community dentist was willing to extract his teeth. But Sandhu safely removed all his upper teeth while taking the necessary steps to ensure proper healing.
Since Stewart is an active member of his community and church, he didn’t want to be without teeth. Sandhu provided “immediate dentures.” Normally, patients have to wait months after extractions to get dentures, but Sandhu’s method – taking a mold of a patient’s teeth before the extractions and sending it to a lab to create the dentures – allows patients, including Stewart, to have a full set of teeth right away.
Living with side effects
Jacks celebrates radiation’s life-saving potential even as she bemoans its lingering effects. “Radiation techniques have improved over the years, but the amount of saliva our patients can produce, after radiation, is always decreased,” she said. Chronic dryness increases the chance of radiation caries, a type of tooth decay.
Patients with reduced saliva flow will need to be on a special oral hygiene regimen for the rest of their lives. That likely includes a high-fluoride toothpaste, since fluoride strengthens teeth against bacterial attack.
For patients who have undergone a stem cell transplant when their donor wasn’t related to them, the donor cells may attack the patient’s cells. That’s called graft versus host disease, and it can lead to severe dry mouth, and, more importantly, raise the risk of oral cancer. Again, the answer is an oral hygiene regimen they’ll maintain for life.
If patients need radiation and chemotherapy, it gets even more complicated. “We recommend those patients have a feeding tube inserted before we start treatment because the likelihood of us needing it is so high,” Jacks said. “We don’t want to delay treatment, nor do we want patients becoming malnourished during treatment.”
Cancer and dental clearance
What to expect if you need clearance before starting cancer treatment
Rarely is anyone excited to see a dentist.
And dentists know that. “More than 90% of patients I see have poor dental health – usually because they have severe dental anxiety,” said Dr. Shaiba Sandhu. “Some will tell me they haven’t seen a dentist in over 20 years.”
Her first order of business is often calming patients’ nerves. Sandhu always begins by outlining for patients what’s entailed in the clearance exam. Understanding what’s going to happen takes the fear out of it.
In 2025, she hopes to offer nitrous oxide sedation – also known as “laughing gas” – to help with anxiety for her Novant Health patients. But until then, if a patient requires more than a local anesthetic, she schedules them at HPU's dental office in Asheboro, where she practices once a month. That’s where she performs extractions, including surgical ones, under nitrous oxide sedation.
She also has operating room privileges, allowing her to perform full-mouth extractions under general anesthesia, if needed for dental clearance. But she adds, “My bar for taking patients to the operating room is very high, as general anesthesia has its own risks. I complete the majority of dental clearances in the outpatient clinic.”
The clearance process starts with a panoramic X-ray, which is done in a hospital and covered by medical insurance. A day or so later, patients meet with Sandhu for a dental evaluation to create a treatment plan focused only on medically necessary care.
During the second visit, treatment begins, which may include dental cleanings, extractions of non-salvageable teeth and the application of silver diamine fluoride (SDF) to halt decay when necessary. “SDF acts like an antibiotic,” Sandhu explained. “It’s applied to the decayed area of the tooth, where it kills the bacteria.”
She does everything that’s needed in one visit in order to get her patients into their cancer treatment as soon as possible. “Because of the time sensitivity involved,” Sandhu said, “my clearance patients are always my top priority.”

Providing this access to care could not be accomplished without our generous supporters. The collective generosity of meaningful giving allows Novant Health to care for more patients across our footprint, provide new equipment, support team member development and assist community members.
If you’d like to join us in making a difference, visit SupportNovantHealth.org/Give-Where-You-Live to learn more.












