When Deanna and Shane Hayes got married in July 2024, they had no idea the next year would bring a miraculous pregnancy, a stunning ultrasound, an emergency C-section, losing their precious daughter Abigail, or spending months in the neonatal intensive care unit.
They also didn’t anticipate how they’d learn to trust a plan bigger than their own.
One surprise … then another
Deanna and Shane both work for Novant Health Forsyth Medical Center — Deanna as the manager of infection prevention and Shane as a public safety officer. They were introduced by Shane’s sister, who also works for Forsyth Medical Center.
Deanna grew up with 15 siblings — not a typo — and hoped to build her own family after getting married. Doctors had cautioned her that her PCOS would make conceiving difficult or even impossible, so she was shocked when just one round of an ovulation-inducing medication a few months into marriage resulted in two pink lines.
Shane came home from work to Deanna holding a sign that read, “We’re having a baby!” Then an ultrasound tech delivered another surprise: They were having three babies.
Shane threw himself into researching minivans. Deanna ran the numbers on diapers and baby gear times three. (“A definite kick in the butt,” she said.) And the couple shared the news with family, who thought they were joking until they saw the ultrasound images.
Holistic care for high-risk pregnancies
‘You aren’t leaving’

At first, 33-year-old Deanna’s pregnancy was smooth sailing — she didn’t even have morning sickness. But at 22 weeks and 6 days, the risks of a multiples pregnancy caught up with her. During a transvaginal ultrasound, Deanna’s doctor noticed her cervix was partially dilated and sent her straight to Forsyth Medical Center.
When the cervix dilates early, babies can be born too soon. And every day of development in utero counts. Babies born at 23 weeks have a 20% to 30% chance of survival. By 24 weeks, it’s 50%, and by 25 weeks, roughly 80% of babies survive.
The team told Deanna that staying in the hospital for monitoring until delivery was her best shot at keeping everyone healthy.
Eager to preserve her parental leave for when the babies arrived, Deanna worked from her hospital room. Except for the day the couple had to discuss with a NICU nurse practitioner what could happen if the babies were born too early.
“When I was a resident back in the 1980s, we didn't resuscitate babies less than 24 weeks old,” said Dr. Thomas Payne, medical director of the neonatal intensive care unit. Back then, a 24-week-old baby only had a 20% survival rate. Thanks to research and technology, survival rates have gone up substantially, but there’s still a high risk for complications when babies are born this early. Sometimes, even the most skilled medical team cannot save a baby facing multiple complications.
The conversation was difficult, Deanna said, but the couple appreciated the chance to ask questions and prepare themselves for all the possibilities. This would serve as a small mercy later.
May 8, 2025: The babies are here!
About two weeks later, Deanna began having contractions. She was 24 weeks and 5 days pregnant. On May 8, her water broke and her cervix thinned enough that a doctor could feel a baby, so they rushed her into surgery to deliver the babies via C-section. The couple had the babies’ names ready: Abigail, Briella and Carter. (“A, B and C,” their parents cleverly decided.)
As they pulled the babies out, the team discovered that each baby had their own placenta (called a trichorionic triplet pregnancy). They also discovered that Abigail’s placenta had detached from the uterus prior to delivery, which meant she had been lacking oxygen and nutrient supply.
Briella and Carter were 1 pound, 4 ounces and Abigail was 1 pound, 1 ounce.
Shane cut Briella’s umbilical cord and was about to check on Deanna when the team told him in an urgent tone: We’re taking Abigail to the NICU, and you need to come with us.
“That felt like I was getting torn in half,” Shane recalled. “Part of me wanted to be there with Deanna — she had just undergone this whole surgery and was super emotional because of the emergency situation. And yet my daughter's fighting for her life.”
Once Shane left, the NICU manager explained to Deanna that Abigail probably wasn’t going to survive. Although Deanna wanted Shane at her side in this devastating moment, she responded as a mother: One of us needs to be with her.
Abigail Rachel Hayes
Abigail had a hole in her lungs, straining her breathing and putting pressure on her heart. The team had been doing chest compressions on Abigail for 30 minutes. They asked Shane: Should we try a chest tube, even though it probably won’t save her? He asked them to go ahead.
But as he held Abigail’s hand and prayed over her, her heart stopped beating. The team called off the tube and encouraged Shane to hold his daughter.

“It definitely was one of my worst mornings for sure, but also a great morning,” Shane said. “It’s so hard to explain the emotions that I was going through — I’m walking past Briella and Carter as I'm carrying Abigail away from her bed. I have two beautiful babies that are stable at that point, and I'm holding their sister who just passed away.”
For her part, Deanna takes comfort knowing that Abigail was with her dad in her last moments. Another mercy: By the time Deanna found out that Abigail had passed, Shane’s parents were at the hospital and her parents were on their way.
“We were trying to figure out how to move forward. How do we mourn Abigail, but still be happy and present with Briella and Carter and give them the love they need?” Shane said. “It was a lot of prayers, a lot of asking for peace and guidance, and a lot of us just being together.”

The labor and delivery team helped, too. “They’re there to celebrate the births, and they’re compassionate in helping families deal with loss,” said Payne, the NICU medical director, adding that helping grieving families is one of their highest callings.
The labor and delivery manager made ink footprints and a cast of Abigail’s foot, and a team member took pictures “so the family will always be able to remember holding their baby,” Payne said.
The Hayes family buried Abigail in their church cemetery and visit her each Sunday. Her headstone reads, “Safe in the arms of Jesus.”
Briella and Carter Hayes
The couple was grieving, and yet they also had reason to rejoice: Briella and Carter were still fighting. Which was good, because they were so premature that they hadn’t developed many essential capabilities.
“A baby born at 24 weeks isn’t going to want to nipple feed — suck, swallow, breathe — for 10 or 11 weeks. That’s two to two and a half months that we have to tube feed them,” Payne said. “We’re trying to use their intestines before they’re meant to be used. And their lungs, eyes, brain, intestines and immune systems are all immature.”

The babies needed to be held and moved in very specific ways to avoid intraventricular hemorrhage and eye disease. They were supported by breathing tubes and feeding tubes. They were highly sensitive to overstimulation. And they didn’t even cry.
Any remaining hopes of having a “normal” newborn experience evaporated almost instantly. “My first time changing a diaper was on my son through the portholes of his incubator,” Shane said. “I was dodging wires, afraid and terrified of hurting him.”
But a nurse walked him through it — and the next challenge, and the next. Neonatal-perinatal doctor Dr. Neelam Pandhi told them that life in the NICU is a roller coaster. “This is an understatement,” Deanna said. The babies have experienced setbacks, as is expected with babies born this early.
The couple hung a sign above the babies’ cribs to remind them to take it “One day at a time,” and made bracelets with this message for other NICU parents.

And they appreciate the care team’s approach: “They’re very quick to respond, and they’ve been able to treat things before they get bad,” Deanna said. And when it’s good, everyone — doctors, nurses, respiratory therapists, speech therapists and the housekeeping team — celebrates with the couple.
Like the first time Deanna got to hold Briella and Carter. Or the first time Briella cried. “When you lose a little girl as your first child,” Shane said, "not hearing Briella cry for weeks and weeks, not knowing, ’Is she going to be okay, is she going to pull through, she’s still on life support’ — to hear her cry felt like such a big milestone. Her lungs are working properly enough for her to make a sound — it hit me harder than I expected.” (He cried, too.)
They knew they were getting to a turning point on June 16 — Shane’s birthday. Shane had also been a premature baby, born at 2 pounds, 1 ounce, and on Shane’s birthday, Carter not only crossed over two pounds for the first time, but specifically weighed in at 2 pounds, 1 ounce.
“It felt like a message from God: I’m still watching. I’ve still got you,” Shane said. “When I was first born, He was there with my parents, and full circle: I have children in the NICU, and my son weighs the same I did 34 years ago.”
Although the couple has had fears, they’ve also marveled as they’ve watched their children developing “on the outside” instead of on the inside. They’re also awed by everyone’s support. Their church life group has provided meals, cleaned their house, and gotten their nursery ready so they can spend all their free time with the babies.

Working for Novant Health has made their journey a little easier, too: They visit the babies before and after work, and can pop in throughout the day to do some feeds or diaper changes. Shane’s boss has let him spend some of his work time in the NICU, as long as he is available for calls. Payne and Pandhi stop by Deanna’s office regularly to give her updates.
The team “has done more than I would ever expect or imagine doctors or nurses to do,” Shane said. Deanna adds, “We have a joke that the nurses try to compete over who’s our favorite. There’s lots of favorites.”
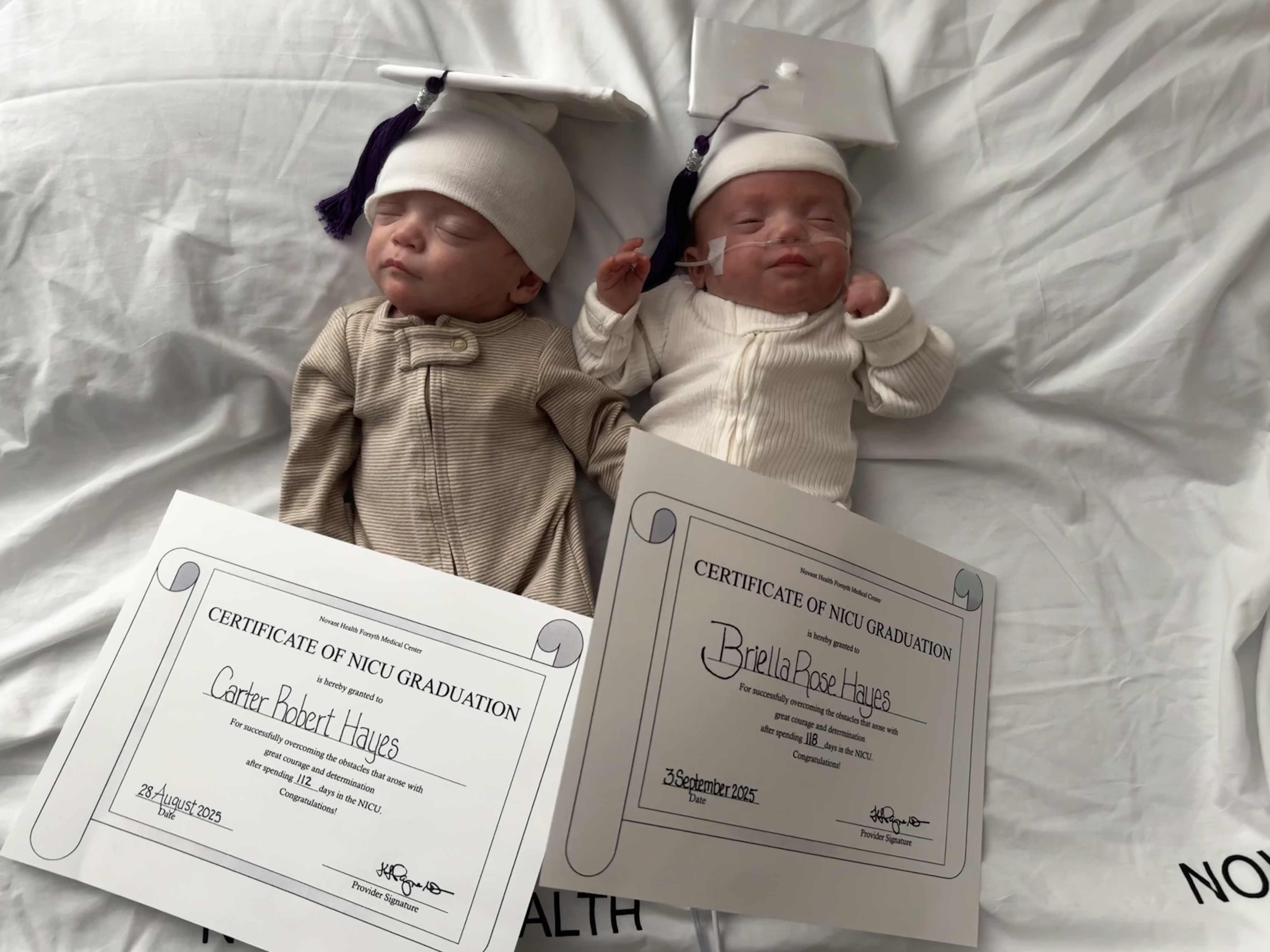
On Aug. 28, Carter left the NICU after 112 days. Just a few days later, the family pushed a double stroller down the hospital hallway to cheers and the wave of pom-poms: After 118 days in the NICU, Briella was going home, too. She’s still on oxygen for now, but she’s home.
Shane is now a stay-at-home dad. They’re still taking it one day a time. But everyone feels good about the direction they’re heading.









