Dopamine is an essential brain chemical known for making us feel good. But for the 1 million people in the U.S. with Parkinson’s disease who don’t get enough dopamine, that deficit can cause tremors and gradually impair the ability to walk and speak.
The progressive movement disorder is the second-most common neurodegenerative disease behind Alzheimer’s, and has no clear cause or cure.
A movement disorder specialist (MDS) can offer patients hope and resources for improved quality of life. With more training than a general neurologist in movement disorders, specifically Parkinson’s disease, an MDS works with patients to develop personalized approaches to surgical interventions, medications and other treatment options.
Holistic care for movement disorders.

“Every Parkinson’s patient has their own specific journey, and each journey can be hard to predict,” said Dr. Rebecca Pratt, a movement disorder specialist who joined Wilmington’s Novant Health Neurology in August. “An MDS trains to know the differences between the many specialized treatments and surgical interventions, and is there with the patient throughout the entire process.”
Advancements in treatment options and research
How soon after a diagnosis should someone see an MDS? While there is no one correct answer, Parkinson’s patients are usually diagnosed in their 60s and referred by a general neurologist.
Meeting with an MDS at least once a year can provide patients greater access to advanced treatment for the effects of Parkinson’s disease, including involuntary movement disorders like dystonia (painful muscle contractions), and dyskinesia (involuntary body movements).
Parkinson’s affects a person’s independence and mobility, but advanced medicines and treatments can extend both for longer, Pratt said. An MDS can help patients assess their needs for both short- and long-term specialized care to improve mobility, including:
Advanced surgical treatment: An MDS has a deep knowledge of procedure options, including whether a patient is a candidate for deep brain stimulation or a less-invasive focused ultrasound.
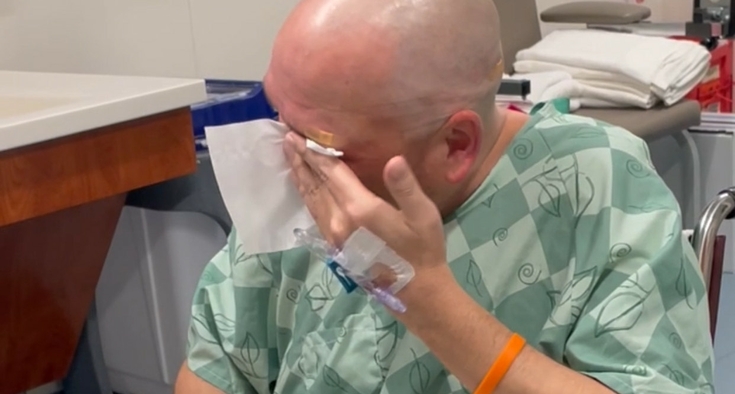
- Deep brain stimulation helps manage symptoms like tremors and stiffness by correcting abnormal brain activity through electrodes implanted into the brain. The implant surgery is performed while the patient is awake during a procedure that takes less than an hour. An implanted pulse generator — which is a device similar to a pacemaker — is placed under the skin in the chest, typically near the collarbone, and connected to the electrodes through a wire under the skin.
- Focused ultrasound is used to reduce tremors by precisely heating and destroying specific areas of the brain. The surgery does not require general anesthesia and has a high success rate. It is a low-risk outpatient procedure that involves no incision, though claustrophobic patients might not be candidates.
- Medications: An MDS navigates the nuances of adjusting drug regimens, anticipating side effects and providing support throughout the patient’s health care journey.
“There are a lot of newly available medicines, mostly centered around dopamine, to also control non-motor symptoms like cognitive impairment, low blood pressure, constipation or difficulty urinating,” Pratt said.
In 2024 the U.S. Food and Drug Administration approved the extended-release formulation Crexont, as well as a small, portable pump that delivers the drug Vyalev (a liquid form of levodopa) to increase dopamine levels. Similar to an insulin pump, this device provides a dose on command to avoid meditation wearing off throughout the day.
Research and clinical trials: Novant Health is recruiting patients to participate in a clinical trial for Vyalev, with a nationwide trial underway.
‘A people person’ with her patients
Even as a kid, Pratt knew she would one day work with patients.
She remembers being about 10 and accompanying her grandfather to his back surgery appointment. When the neurosurgeon brought up the topic of deep brain stimulation surgery, Pratt was hooked.
“I thought it was the coolest thing I’d ever heard,” she said. “That’s when I knew I was going to be a brain doctor.”
Much of the role requires putting patients at ease by building trust. For Pratt, that means encouraging them to ask a lot of questions.
“Otherwise, that’s how things can get missed,” she said. “I try not to use a lot of doctor-speak because it’s not a good way to connect with a patient. I’m very much a people person.”
In the meantime, are we closer to a cure for Parkinson’s?
“That’s a difficult question to answer, but we are making progress,” Pratt said. “I hope the answer is yes, though figuring out the cause may not lead immediately to a cure. A lot of stem cell research trials are still in the early stages, but they are promising.”
Staying active is key to slowing progression
Regular cardiovascular exercise — like going for a run or brisk walk for a half-hour each day — is essential for improving both motor symptoms, like gait and posture, and non-motor symptoms, like low mood. Exercise also may slow disease progression, studies show.
“In terms of which exercise plan is best, whatever you are going to enjoy the most or what works into your schedule is what I recommend,” Pratt said.
Because Parkinson’s disease is progressive, meaning it changes over time, helping patients anticipate and adapt to mobility changes is a challenge unique to each patient.
“It’s helpful to explain to patients that Parkinson’s does not significantly change their lifespan,” Pratt said. “Most of the time, that’s the worry: ‘Is this going to be fatal?’ But the answer is almost always no.”
In addition to discussing ways to avoid being sedentary, an MDS also guides patients through therapeutic options:
- Physical therapy: Provides one-on-one recommended exercise regimens and incorporates assistive devices like canes or walkers as needed.
- Occupational therapy: Encourages fuller movement while working to strengthen daily tasks like brushing teeth, buttoning a shirt, putting on makeup or writing with a pen.
- Speech therapy: Addresses swallowing difficulty and helps overcome challenges with speaking, enunciating and voice projection.
Free exercise class in Wilmington brings strength and support to individuals with Parkinson’s disease
By Susan Miller
Exercise is important for improving neurological function and muscle movement in individuals with Parkinson’s disease. That’s why the Novant Health Foundation has partnered with Beat Parkinson’s Today to offer an exercise class in Wilmington for individuals with Parkinson’s disease, free of cost to participants.
Dr. Rebecca Pratt, a Novant Health movement disorder specialist, recommends Parkinson's-specific exercise classes for her patients because the group format helps attendees stay motivated.
“Apathy or lack of motivation is really common with Parkinson's disease because that part of the brain is closely related,” Pratt explained. “I usually ask patients to get involved with exercise classes because they provide an external motivator to stay active.”

The 1-hour class uses Beat Parkinson’s Today’s research-based workout format, incorporating high-intensity interval training. Movements like squats, wall sits, sit-to-stands (sitting down in a chair and standing up without using the hands for support), lateral lunges and boxing cross-jabs all help improve balance, coordination, strength and mobility.
Priss Endo, 79, has committed to working out ever since she received her Parkinson’s diagnosis 1 1/2 years ago. Two unexplained falls led to her diagnosis, and exercising in the Beat Parkinson’s Today class is helping her regain stability and fluidity of movement.
“What they say is ‘motion is lotion,’ and that’s true,” she said.
Bob Corriston, 86, agreed. While he walks with a cane, he’s noticed a big change since he began attending the class.
“I mostly just carry the cane now,” he said.
The class instructor, fitness trainer and certified strength and conditioning coach Carlie Haase, explained the science that’s applied in each class: exercise enhances dopamine production, which in turn supports brain neuron function and survival. Plus, she said, there’s the bonus of camaraderie, talk and laughter with other classmates.
“It’s so much fun,” she said.