Your heart rate, or pulse, is a vital sign taken every time you visit your doctor. And those beats per minute say a lot about your overall health.
A low heart rate could indicate the need for a pacemaker, which acts as a metronome for your heartbeat. Its purpose: to correct an abnormally slow heart rhythm.

The tiny battery-operated pulse generator, about the size of a silver dollar, is implanted under the skin and uses leads, or wires, and electrical impulses to keep the heart rate and rhythm steady and strong. The procedure, done under anesthesia, takes about an hour with the patient typically going home the same day, said physician assistant Garrett Bostwick of Novant Health Heart & Vascular Institute in Wilmington.
In 2025, Wilmington’s Novant Health Heart & Vascular Institute began offering Aveir, a wireless pacemaker that requires no chest incision. For qualifying patients, the option offers an alternative when a traditional pacemaker isn’t the best fit, Bostwick said.
While attending Wake Forest University, Bostwick “fell in love with cardiovascular medicine,” he said. “I had a lifelong gravitation toward the sciences and later developed a love for the physiology of the body and the heart.”
Here, Bostwick explains how they work together and answers common questions about a pacemaker’s role in maintaining a smooth, consistent heart rate.
Take the first step toward improving your cardiac health.
Who qualifies for a pacemaker, and how do I know that I need one?
People who need a pacemaker have a heart that is not beating as fast as it should. Sometimes people with chronically low heart rates experience symptoms like lightheadedness, fatigue or shortness of breath. Pacemakers are most commonly needed for patients in their 60s, 70s and 80s, and that need can be identified during a routine visit with your primary care provider.
How fast should my heart be beating?
A textbook normal resting heart rate — such as when you’re sitting and watching TV — is typically anywhere from 60 to 90 beats per minute. (Editor’s note: Think of a tempo somewhere between “My Girl” by The Temptations and “Shoop” by Salt-N-Pepa.)
While there’s no exact number, people with heart rates consistently measuring below that threshold (and especially those with associated symptoms) can be candidates for a pacemaker.
A pacemaker is one device in a range of implants that address heart issues. What’s the difference between them?
Both a pacemaker and a defibrillator address heart rhythm-related issues. But while a pacemaker can only correct abnormal slow heart rhythms, a defibrillator can pace the heart and address both dangerously slow and fast rhythms.
The Watchman heart implant helps reduce stroke risk in atrial fibrillation (AFib) patients who cannot tolerate blood thinners. (AFib is the most common heart arrhythmia.) The Barostim device implant does not control heart rhythm, but stimulates blood pressure sensors to address heart failure.
How is it determined that someone needs a pacemaker?
There are people with emergent, life-threatening situations — like an abnormal heart rhythm — who need a pacemaker on the spot. (Editor’s note: Here’s an example of that with Wilmington marathon runner Peyton Chitty.)
There are people who don’t need pacemakers because their heart rate is fine. And then there are people in between who have slow heart rates or rhythms only intermittently. It’s that gray area where a discussion between the cardiologist and the patient should determine whether a pacemaker will help.
Is it OK to get wet after undergoing pacemaker implant surgery?
Immediately after an incision and implant, there are some restrictions with showering or swimming for those first few weeks. But after the incision heals, the device is completely contained within the body and you’re free to go underwater.
We encourage our patients to remain as active as possible. There are no specific activity restrictions or things to avoid, but there can be some pacemaker interference with external devices. That means avoiding going through metal detectors at the airport. Beyond that, most day-to-day electronics are safe to use. (Editor’s note: The Transportation Security Administration recommends advising your TSA agent at the airport that you need alternative screening.)
How long does a pacemaker battery last, and can I feel it?
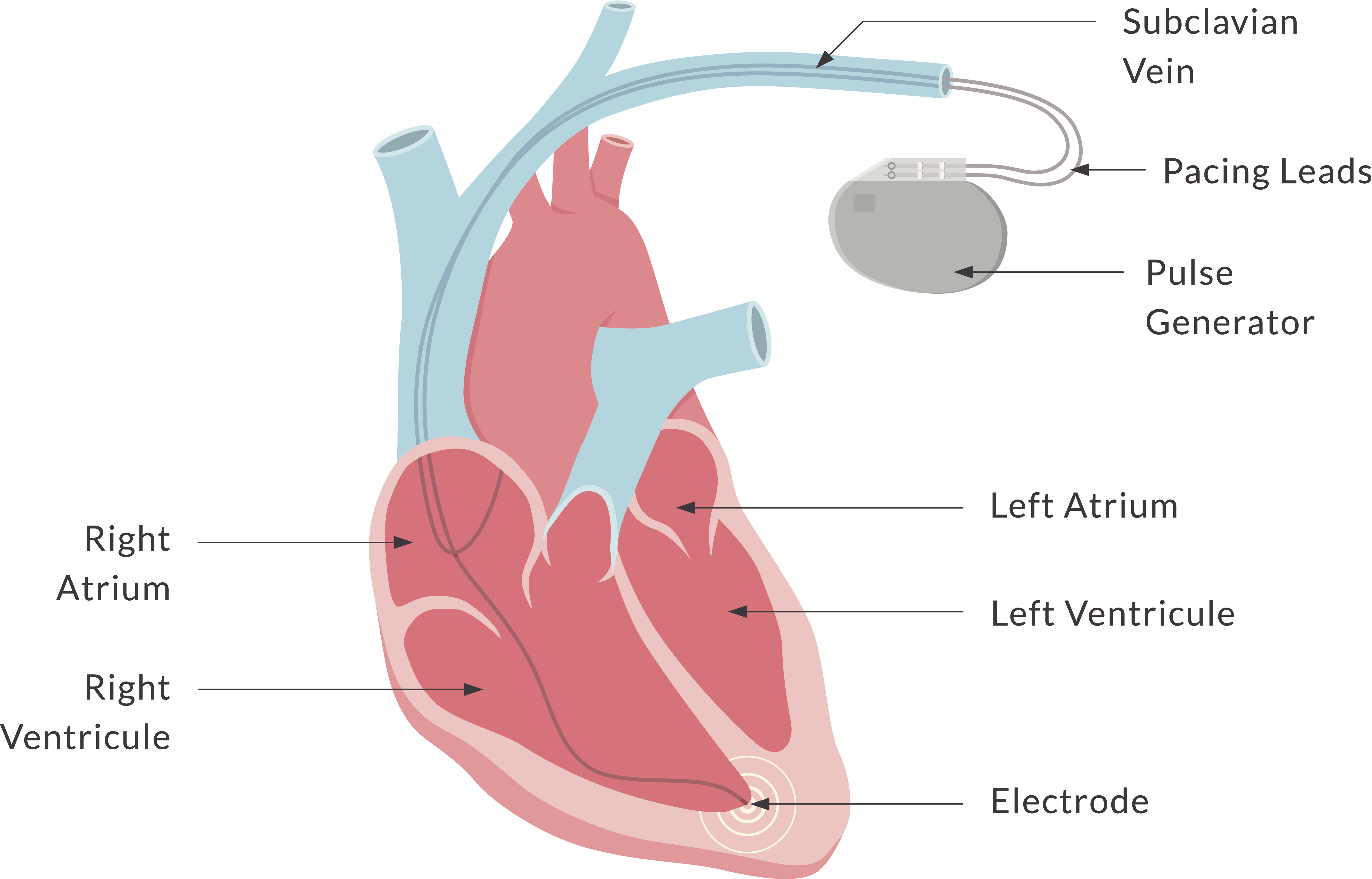
On average, about 10 years. The pulse generator with the battery inside resides just underneath the skin, below the left clavicle. The battery within the pulse generator cannot be replaced by itself. We must replace the whole system, minus the wires, when the battery runs low.
Sometimes you can see a faint outline of the pulse generator. But within six months or so, most patients forget it’s even there. Following surgery, we check in with the patient at least once a year and remotely monitor every pacemaker. So even if you’re not seeing us in person, we’re checking on your pacemaker intermittently throughout the year.
What should patients expect from recovery after pacemaker implant surgery?
People generally bounce back quickly. There’s usually some soreness for up to five days, but because it’s a same-day procedure for most patients, we expect that patients will do just fine at home on their own. But it’s important to adhere to the temporary post-procedure restrictions (no swimming or heavy lifting) for several weeks.













