Most nurses chose the field to help people recover from an illness or injury, to help people get better.
Monique Chatman’s job is a little different. Her goal is to help patients feel better.
She’s a family nurse practitioner at Novant Health Presbyterian Medical Center, where she specializes in palliative care. Her patients have life-limiting or serious illnesses. She’s there to help them find a path through complex medical choices and arrive at a quality of life that gives them peace.
Palliative care and hospice care. What’s the difference?
Palliative care is focused on improving the quality of life for patients with serious illnesses.
Hospice care is for individuals with a prognosis of only days or months to live and curative care has stopped.
Palliative care continues to grow at hospitals across the U.S. and is an important part of Novant Health’s commitment to treating the whole patient. And Chatman works closely with other care team members who strive to help patients find the best way forward.
Chatman’s patients include anyone hospitalized at Presbyterian Medical Center with a life-limiting or serious illness – conditions such as COPD, end-stage renal disease, heart failure and what she sees most often: cancer. And she’s ideally suited to help cancer patients. A few years ago, she was one herself. (See more on this in the sidebar below.)
Chatman had been a nurse for nine years when she returned to school to become a nurse practitioner, a field that allows nurses to be more deeply involved in treating patients. (In the medical field, they’re sometimes referred to as advanced practice providers, or APPs.)
It was her work at Novant Health Matthews Medical Center in a palliative care/oncology unit that led her to discover a passion for end-of-life care. After graduate school and a one-year fellowship, she returned to Novant Health in 2017, this time to Presbyterian.
Our palliative care services focus on providing the best quality of life.
Learning from personal experience
While she was undergoing her treatment for cancer, she took a break from seeing oncology patients because it could be triggering. “I had thoughts of: Why me? And they persisted even after my treatment,” she said. “I began wondering: Why did I survive when young mothers with little children at home didn’t?”
During treatment, “I didn’t want to talk to anyone about it,” she said. “I just wanted to get through it and be done. I was already in therapy; I had a counselor – but not one who specialized in oncology. And I hadn’t been around other people who could relate to what I was feeling. I wanted to support other survivors who finished their treatment and wondered: What next?”
And that gave her an idea: What if she could help start a post-treatment survivorship group at Novant Health? She talked to her manager, Eva Rodriguez, about creating one. And along with Chelsea Mitchell, a Novant Health chaplain; Tiffany Young, a licensed clinical social worker (LCSW) at the Novant Health Cancer Institute Kemp Bessant Support Center; and Debbie Smith, an LCSW at the Novant Health Huntersville Cancer Institute, she did.

The first meeting was held over Zoom in February 2024. Since then, the group has met every other month, and the session is offered, at no charge, in person and virtually. To learn more, visit the group’s Facebook page, call 704-384-3513 and see the footnote at the bottom of this story.
Patients must be no more than two years out from treatment. “Typically, it’s within those first couple of years that people have the most challenges,” Chatman said. That’s more than a statistic she read. She lived it. “It took me a while to consider myself a survivor,” she said.
While researching for the support group, she came across a quote: You’re a survivor at the time of diagnosis.
“I had never thought about it that way,” she said. “It was around that time I started to accept that cancer was an unfortunate thing that happened, yet it’s also something I'm thankful for because it put me in a better position to help people.
“I used to feel like I needed to do something as a survivor – sell cancer T-shirts or something – until a friend who’s an LCSW in the mental illness space said, ‘Monique, why do you feel like you have to do something? Just being here is doing.’ That thought totally shifted my mindset.”
At the bedside
Her own battle with a scary disease helps her in the work she does daily.
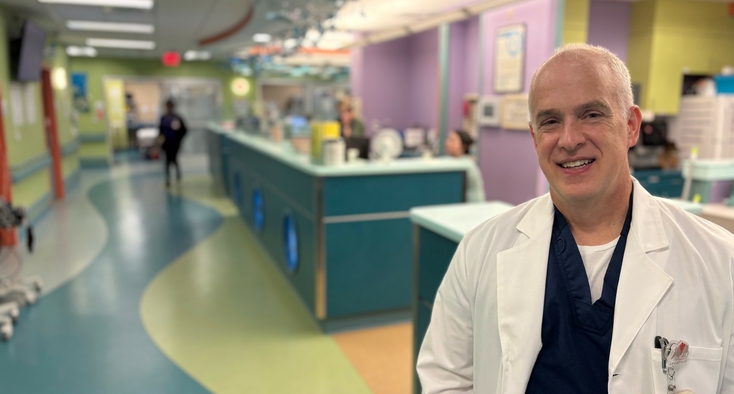
Coursing the halls of Presbyterian Medical Center, Chatman brings a quick smile to the bedside, where she’s careful and calm in laying out the daunting options patients sometimes face.
Patients are grateful to Chatman and the entire team for helping them figure out these difficult decisions. One patient recently treated the whole team to pizza and Chick-fil-A to show his appreciation.
When life ends soon after it began
Chatman also sees patients at Novant Health Hemby Children’s Hospital, housed within Presbyterian. “Sadly, life-limiting illnesses can happen at the beginning of life,” she said. “They can even be diagnosed in utero. But those parents still have hopes for their children.”
The parents of a baby with a genetic heart condition born close to the holidays wanted Christmas pictures of their infant. Other parents want a baptism. “It’s about identifying what’s most important to the parents and then trying to find the best way to carry that out,” Chatman said.
She doesn’t do that alone. On her team are a physician, three nurse practitioners, a nurse navigator and a social worker. She’s in frequent contact with the chaplain’s office, and her colleagues also include the attending physicians and nurses treating patients with life-limiting or terminal illnesses.
Her manager believes cancer made Chatman bolder. “Cancer seems to have made Monique more open to new opportunities she may not have considered before,” Rodriguez said. “Working with pediatrics and the support group are two examples. She might’ve hesitated a little before, but now she embraces new things.”
Dealing with the heavy stuff
Chatman’s work is rewarding but also draining. So, she’s careful to equip herself with all the tools she needs.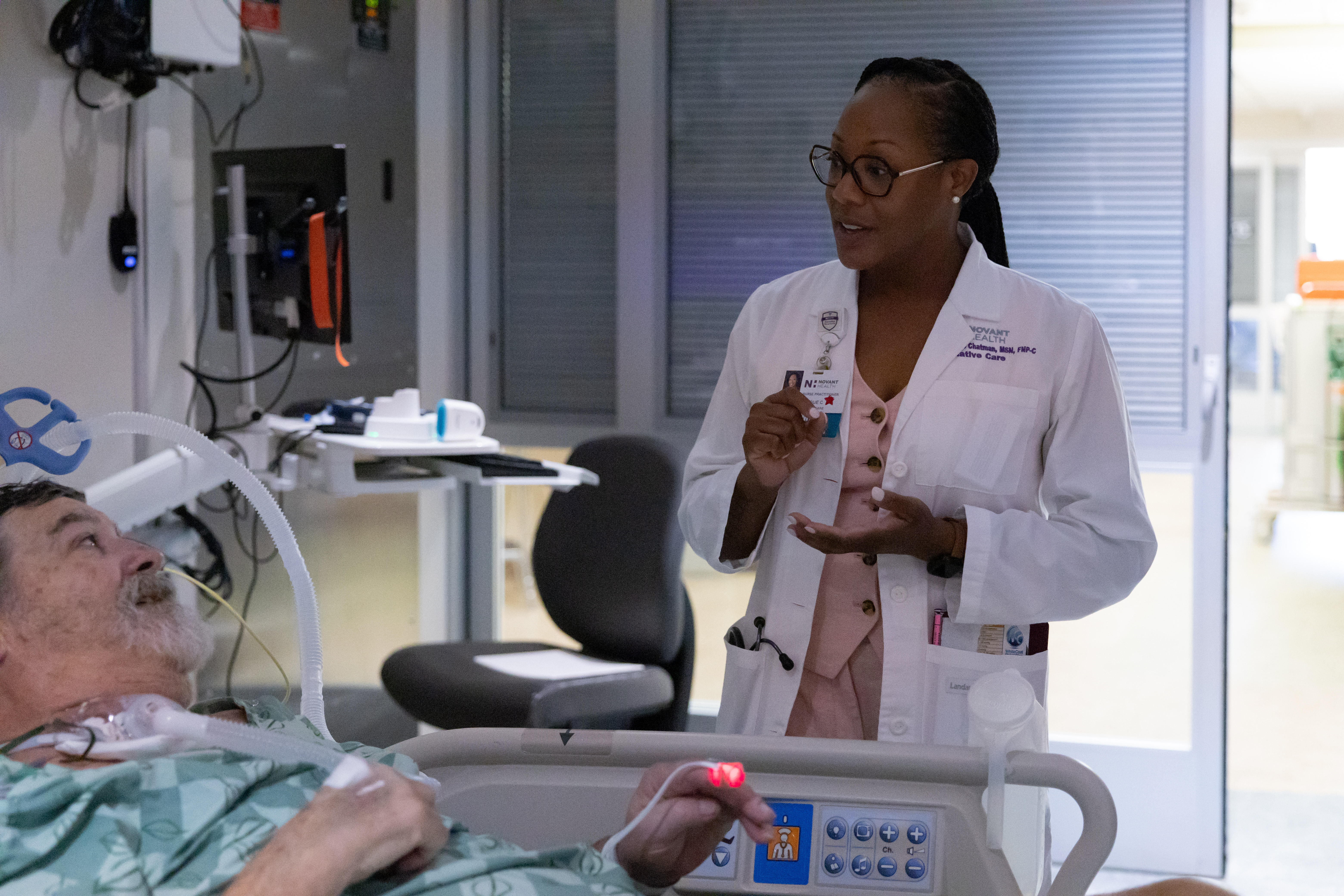
Chatman’s work is rewarding but also draining. So, she’s careful to equip herself with all the tools she needs.
She works out and leans on her faith; her network of family and friends; her team, including its leadership; and her love of travel. “I’m single with no children, and travel is something I always look forward to,” she said. “I usually plan a few trips a year.” She went to Aruba earlier this year and is planning a nature-focused trip to Costa Rica in September.
Having boundaries helps, too. “When I leave work, I leave my day behind,” she said. “We have a good team, and we discuss our feelings with each other. So, in a sense, I release that energy before I even leave work.”
Cancer blurred the lines between Chatman’s personal and professional lives. It enhanced what Rodriguez called “her natural ability to connect with patients and their families” that makes Chatman so good at her job.
“I'm a cancer survivor caring for cancer patients,” Chatman said. There’s power in that for both patient and provider.
Support for post-treatment cancer patients wondering: What now? Monique Chatman helped start a support group for cancer survivors. Meetings are held on Zoom from noon to 1 p.m. on the second Tuesday of every other month. The next two are on Aug. 14 and Oct. 9. There’s no charge to attend, but you’ll need to register in advance by calling 704-384-3513. You’ll receive a meeting ID and password to join.
A ‘deeper level of understanding’
Cancer added another dimension to palliative care nurse practitioner’s work
Monique Chatman had been a palliative care nurse practitioner for three years when she got her own cancer diagnosis: Stage 2 ampullary adenocarcinoma, a rare cancer of an area in the small intestine called the ampulla. In 2019, she had surgery to remove a tumor on her pancreas. Part of her small intestine and stomach were also removed during the complex and invasive procedure called Whipple surgery.
She praises her Novant Health care team, which included oncologist Dr. Dipika Misra; gastroenterologist Dr. John Gardiner Roddey (“His recommendation to have frequent scans is what found the cancer”) and radiation oncologist Dr. William Warlick.
Six months of chemo followed surgery. Chatman stayed active and continued working during her treatment because her oncologist told her, “The people who do the best are those who don't stop.”
The only days she didn’t work were the days she had chemo.
Radiation, which she had in January 2020, didn’t slow her down, either. Her office and the radiation department are in the same building. She’d go there at 8 a.m. for treatment and be at work by 8:30.
Treatment left Chatman with the same side effects many of her patients experience – hair loss, neuropathy, peeling skin, fatigue.
But cancer came with positive changes, too. Her manager, Eva Rodriguez, said, “Monique has grown a lot as a provider since her cancer experience. I knew she was well-suited to this work before, but cancer heightened her natural abilities.”
Chatman said being a cancer survivor has “strengthened my empathy. There's this deeper level of understanding now. If someone is feeling fatigued, experiencing neuropathy, if they're nauseous – any of those – I definitely understand, because I was once there.”