If you’ve ever found yourself too busy to take care of your own health, Dr. Robert Beam understands. The MD with a PhD and an MBA has always burned the candle at both ends.
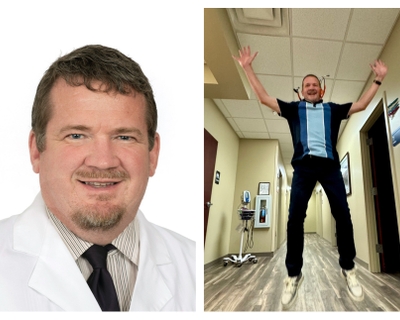
In August 2024, he joined Novant Health Northern Family Medicine in Greensboro as lead clinician. He’d gained weight while working from home for 12 years and didn’t want to discuss weight loss with patients without taking his own advice. He set his mind to dropping the nearly 50 pounds he’d put on and did it without medication.
He also — at long last — got a mole checked and learned it was skin cancer.
“It was my own foolishness that caused me to neglect it,” he said. “I saw it daily when I come out of the shower and never did anything about it. It embarrasses me as a physician to say that; I know better. I felt I had some obligation to share my story.”
Beam is unusually candid about what he wishes he’d done differently. This conversation has been lightly edited for length.
Want to start your own journey to better health? We can help.
Thanks for talking about your two recent health challenges. Which should we start with?
Melanoma; it’s the only skin cancer with a significant mortality rate. Mine was found at Stage 1 when there’s a 10-year, 96% survival rate. So, I don’t want to steal valor from those who’ve gone through significant peril; there are people who have been through much worse.
I always have my annual physical. My colonoscopy is up to date. My blood work looks good.
I also work a lot. I've been with Novant Health for 12 years. I started in urgent care, which is a 7-day-a-week job. I was always filling in when there was a need. I worked my way up to medical director and used my busy schedule and my desire to serve the community as an excuse for never seeing a dermatologist.
I’d seen this mole on my shoulder for 10, maybe 15, years and would think: I should get that checked. But it didn't bleed, itch or appear to be changing. I got out of the shower one day, saw it and wondered: Have I been staring at cancer this entire time?
Did you have a dermatologist?
I’ve never been to one. But one day, I got an EPIC (electronic health records) message from a dermatologist, Dr. Deborah Dorrell, about a patient I’d referred. I asked if I could send her a picture of my mole. She arranged for me to be seen two days later, which I thought was just professional courtesy.The biopsy was on a Friday. I saw the results on MyChart the following Wednesday: Malignant melanoma. For someone used to delivering bad news, it was hard to be on the receiving end.
The more I read, the more I realized the insidious thing about melanoma is that it can spread without you knowing it. It can skip through lymph nodes and show up in other places in the body.
With most cancers, if you're cancer-free for five years, you're considered cured. With melanoma, 10 years is considered the cure point. Even with Stage 1 melanoma, there are 3% to 4% of patients who don't survive 10 years. Those are great odds for a gambler — less so for a pathology report.
The likelihood this will spread is incredibly low. Logically, I get that. Emotionally, that’s another story.
How was your melanoma treated?
With Stage 1 melanoma, there's no chemotherapy and no radiation. Keytruda, an immunotherapy drug used to treat some cancers, is available for later stages.
To remove Stage 1 melanomas like mine, they do a wide-area excision and take out several inches around the cancer to try to get any potential microscopic spread. I also had plastic surgery — performed by Dr. George Lawson of Forsyth Plastic Surgery — under general anesthesia to take out a small section from the front of my left shoulder.
You can opt to have a lymph node biopsy — a bigger surgery with its own risks and complications. I met with a cancer surgeon, Dr. Scott Berger of Novant Health Salem Surgical Associates - Winston-Salem, who didn’t think it necessary. I did my own research and concluded the same thing, although a small piece of me wonders if I’ll regret this.
But you have to be careful not to overreact. At this point, I’m presumptively cured, but I’ll see a dermatologist every three months for evaluation.
Has having a serious cancer changed the way you practice medicine?
It’s definitely changed the way I deliver information.
When I began telling people about my cancer, some folks told me they knew how I felt because they had had a basal or squamous cell carcinoma. Those almost never spread. At first, I felt I had to explain how lethal melanoma can be. But I didn’t like the sound of “My cancer’s more serious than your cancer.”
Then, I realized: To them, theirs was just as serious. When you hear the word “cancer,” you think the worst. Having cancer made me more sensitive about the word “cancer.”
When I saw the message on MyChart, a piece of me thought: Do I cancel the rest of my day and go home? To my dermatology friends and surgeon friends who see melanoma all the time, that probably sounds histrionic.
Here's the reality: We treat everything like it's an absolute, when it’s a statistical probability. I’m sitting in my office 3 miles from my house. There’s no guarantee I'll make it home tonight. The probability is highly in my favor that I’ll make it home and this cancer is nothing more than an annoyance.
I hope so, and I suspect that’s true. Now, about your weight loss …
When I graduated high school, I was 5 feet, 11 inches and 155 pounds. I couldn't gain weight for anything. When I got married 32 years ago, I weighed 165. And then, like most people, I added a few pounds every year. I don't think I realized it.
I was in private practice when I first came out of residency. Seeing patients, doing your own HR —that’s very stressful. I told myself I didn’t have time to eat right. There was often snack food in the office, and I indulged.
So, private practice is when your unhealthy eating habits started?
How he did it
Dr. Beam got comfortable with a little hunger
Dr. Robert Beam and legions of registered dietitians agree: You cannot out-exercise a bad diet.
“For every mile you run, you burn 100 calories,” he said. “Every slice of cheese you eat is 100 calories. Which can you do faster? There aren’t enough hours in the day to outrun a bad diet.”
Weight-loss pills and injections, he pointed out, don’t make you exercise more. They suppress your appetite.
If you're going to lose weight without medication, he said, some people may have to become comfortable with a little hunger.
To be clear: Not all registered dietitians would approve of Beam’s approach of daytime fasting. He eats breakfast and dinner and nothing in between. “I’m at work for 12 hours, and I don’t eat,” he said. “There's no magic to that number. For others, it might be eight hours.”
For the first six months of this major lifestyle change, his goal was to limit — not eliminate — starches, bread, pasta, potatoes, corn and rice. “During that time, I dropped from 212 to 168. And I felt great,” he said.
He calls his breakfast of a protein shake and a cup of yogurt “boring and consistent.” Dinner might be grilled chicken, roasted broccoli and a salad.
He began a new exercise program at the same time he started daytime fasting.
His exercise routine — bench presses, push-ups and pull-ups — is impressive, but he doesn’t credit it with his weight loss.
“As we age, any exercise that builds muscle mass is important and helpful for weight loss,” he said, “not just because the exercise burns calories, but because the more muscle you have, the more calories you're burning while sitting still.”
I think so. I viewed food as stress relief, as a reward for balancing a family — a wife and four young children —with running a private practice. I knew I was making unhealthy choices, but it felt like a necessary compromise in order to be all things to all people. If I have no time to eat, I was justified in eating a fast-food burger.
After I became the medical director for virtual care, I began working from home. In between Zoom calls, the dog and I would walk to the refrigerator. I wasn’t eating poorly — a handful of grapes, a slice of cheese, lunch meat. But it was a constant influx, and my dog, Murphy, wasn't going to tell on me since he was getting his share.
Before starting this job in August 2024, I realized how disingenuous it would be to have conversations with patients about weight loss.
I had the desire to lose weight, but desire isn’t enough. Whether it's smoking, alcohol, gambling, food — whatever the addiction, you also need motivation. My motivation was the embarrassing thought of telling somebody to lose weight while being overweight myself.
How do you maintain your weight loss?
First thing every morning, I climb on that scale. That’s feedback on how I did yesterday. I’ve learned what I can and can't eat, what's a reasonable amount, what's not. If you want to lose weight, you have to confront the reality of yesterday.
The scale going up isn’t always a bad thing. If my boys came over and we ordered pizza and watched a ball game, I chose that. I'm OK with it. But I'm not going to ignore the scale. I want to know what the damage is and own it.
You must have patients who saw you at your heaviest and have noticed your weight loss.
The funny thing is, my Novant Health picture is me before the weight loss. So, when patients look me up online and then meet me in person, they often say I need a new picture.
The way you went about losing weight — do you recommend that to your patients?
I do. And many say, “I don't think I can,” but quite a few leave inspired to try.
I should add, though: I’m not a weight-loss specialist. No one should embark on any weight-loss plan without consulting their doctor or other provider. To be clear: What I did is not for everybody. Also, there are individuals with metabolic issues who have done the right things and still can’t lose weight. But that’s not the majority of us.
The problem with food addiction, or any addiction, is that we don’t believe we can change. But look at individuals with alcohol use disorder who stop drinking and come out the other side. When you see hope, you realize that can be you, too.
Portrait of an overachiever
After college, Robert Beam went on to earn three more degrees
Robert Beam always wanted to go into medicine. But he took a detour first.
“I didn’t have any money,” he said. “I went to the University of Tennessee in my hometown on a partial scholarship. I had majors in zoology, biology, biochemistry and minors in chemistry and physical science, and I was one class short of a minor in religious studies. I knew good grades were my only way into med school. I had good grades, but I was exhausted.
“A professor flattered me into staying at UT, working on a PhD and doing a teaching assistantship. My PhD was in life sciences with a concentration in physiology. Medical research, in other words. After six years researching how a North American chameleon — the green anole — changes colors, I was close to having a PhD but no closer to the career I wanted.”
With encouragement from his wife, Shannon, he applied to medical school at the University of Tennessee in Memphis, seven hours from Knoxville. He was accepted and somehow found time to write his 300-page dissertation during his first year of medical school.
After graduation, he and his family — including son Ryan, now 25; and fraternal triplets, Caitlin, Alex and Michael, now 23 — returned to Knoxville, and he began private practice, which proved a struggle. “I was raised to finish what I start, but sometimes, you have to cut your losses,” he said.
He shut down that practice and started over in North Carolina.
“But something about that closed practice never sat right with my soul,” he said, “and I had to make retribution.”
For a workhorse like Beam, retribution took the form of going back to school for an MBA, which he earned at 56. “I guess I wanted to know,” he said, “that if I ever went into private practice again, I could do it.”












