The Novant Health movement disorders program offers the most advanced therapies for patients with movement disorders. “We work in conjunction with local and referring physicians to provide the most patient-centered care possible, no matter where they’re traveling from,” said Dr. Robert Wiggins, neurologist and movement disorder specialist at Novant Health Neurology & Sleep in Charlotte. “Movement disorders are complicated, but the most effective and advanced therapies allow for hope and optimism.”
Referring physicians can help start this discussion. Whether patients are struggling with Parkinson’s disease, essential tremor or another movement disorder, Novant Health offers deep expertise and multiple approaches that can help restore control and better quality of life for the patients referred to them.

“If medications are no longer keeping a patient's symptoms controlled, and those symptoms are having a significant negative impact on the patient's quality of life, it's a very appropriate time to look at available surgical treatments,” said Dr. Charles Munyon, a neurosurgeon at Novant Health Brain & Spine Surgery in Charlotte.
Focused ultrasound can offer immediate improvement.
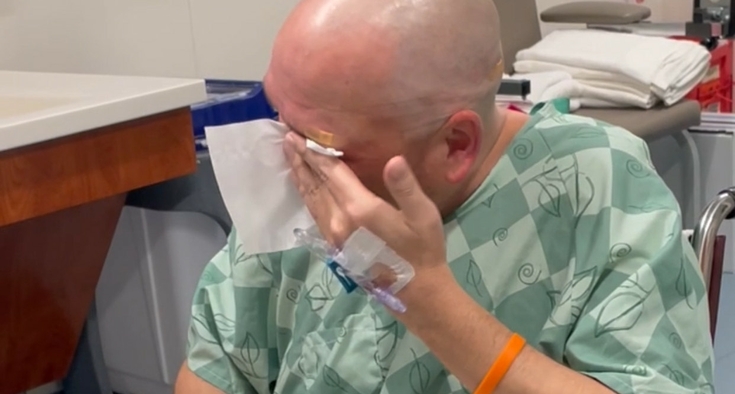
Since September 2020, Novant Health neurosurgeons have performed more than 700 incisionless brain surgeries using MRI-guided focused ultrasound for thalamotomy, the first program of its kind in the Carolinas. Many patients experience rapid improvement, with tremor reduction of up to 90%, often enabling people to eat, drink, write legibly and return to hobbies like art.
“Focused ultrasound works by creating a lesion in the brain, a precise burn made using sound waves under MRI guidance, which interrupts the circuit which is causing the patient's symptoms,” Munyon said. “The treatment typically takes between 45 minutes and an hour, and the effect is instantaneous.”
Deep brain stimulation can offer ongoing fine-tuning.
Novant Health neurosurgeons also offer deep brain stimulation (DBS) as an approach for patients who have medication-refractory tremor, disabling motor fluctuations, intolerable medication side effects, or unpredictable offs, when medication just stops working during the day.
Specifically, DBS offers long-term efficacy, more control and adjustment capabilities based on patient needs, especially when implemented earlier in a patient’s disease course. DBS is particularly valuable for progressive conditions such as Parkinson’s disease or essential tremor.
“There are a number of other conditions for which DBS is sometimes used,” Munyon said, “including dystonia, Tourette's syndrome, obsessive-compulsive disorder, and even certain chronic pain conditions, but these are indications that require very specialized care.”
DBS is a process.
Two procedures are necessary for implanting the two stimulator leads, then implanting the battery and the small, implantable pulse generator (IPG).
Wiggins said, “Two to three weeks after that, we activate the deep brain stimulator in clinic, and patients typically begin noticing symptom improvement. While the idea of having wires placed in the brain can feel daunting, I reassure patients that we use advanced imaging to precisely position the leads for optimal symptom control.”
Once programming is complete, patients can adjust their programmer on their own during the day in a safe range that has been set for them. They can take it up a notch to gain more control when helpful for a hobby or task, or they can bring it down a notch if they are having some side effects of the stimulation.
Then patients will visit their specialist every 3 to 6 months depending on their symptoms. “Follow-up visits enable us to check the battery and programming and ensure the device hasn’t been damaged by an issue like a fall,” Wiggins said. “We also make adjustments to address side effects such as slurred speech, voice changes, or numbness and tingling.”
“We work closely with patients after deep brain stimulation, both in-clinic and remotely in collaboration with their local physician,” Wiggins said. “We’re here to help fine-tune their medications, optimize stimulation settings and connect them with rehabilitation therapies that help maximize function.”
“There are different ways to measure the effects of treatment objectively, but the most important measure is improvement in patient quality of life. “There will still likely be symptoms of the underlying condition, but the goal of treatment is to significantly reduce the impact they have on quality of life.”
It all starts with a referral. “Whether or not DBS or FUS ends up being a useful option, it is always our pleasure to meet with any patient who has questions about their options,” Munyon said. “Patients do not need any kind of imaging prior to referral; we are happy to meet with any patient who wants to discuss treatments that might be available to them.”
Our referral process is designed to save you time and improve patient care by reducing the obstacles you face every day – such as patients waiting weeks to be scheduled, repeated phone calls and unclear next steps.
- Save time. One centralized eFax handles referrals to all our North Carolina specialists.
- Accelerate care. Patients can get from referral to treatment with appointments available in as little as 48 hours.
- Higher patient satisfaction. Our optimized schedules and workflows create more appointment options for a smoother patient experience.
- Reduce administrative burden. Our process frees your team to focus on care, not coordination.
- 24/7 behavioral health. Patients can call 800-718-3550 anytime, with referral outreach within 48 hours.